Bay Area
Orthopedics
Get care close to home. Our orthopedic clinic is supported by a highly skilled team, committed to helping you move better and get back to what you love.
1775 Thompson Rd, Coos Bay, Oregon 97420
(541) 269-8111Top Suggestions
We believe orthopedic care should be clear, complete, and centered on you. Here’s what sets us apart:
Our orthopedic surgeons in Coos Bay are highly trained, board-certified specialists and orthopedic team who provide care for a wide range of orthopedic conditions.
Not sure what’s causing your pain? We treat everything from everyday strains to complex injuries, helping you heal well and move with confidence.
We offer a full range of surgical and non-surgical treatments to relieve pain, restore function, and support your long-term recovery.
Whether its hips, knees or shoulder, we specialize in total joint replacement surgical services. Our Joint Replacement Destination Center was certified in 2017 and is recognized for excellence. This designation provides a better patient experience and superior clinical outcomes through a comprehensive approach to patient care.


Injuries often happen when you least expect them. Our Level III Trauma Center is staffed around the clock with emergency physicians ready to deliver expert orthopedic care when you need it most.
An injury can change your season, but it doesn’t have to end it. Our board-certified orthopedic surgeons and sports medicine team provide expert care and rehab to help you recover and return to the activities you love.


Accurate imaging is the foundation of effective orthopedic care. Our technologists perform over 600,000 procedures each year, with board-certified radiologists delivering expert interpretation and support for our orthopedic team.
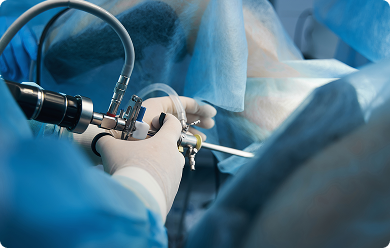
Not every surgery needs a big incision. Arthroscopy is a minimally invasive technique used to examine, diagnose, and treat joint conditions. It offers lower surgical risks, faster recovery, and a quicker return to the things you enjoy.

Surgery isn’t the first or only option. Our specialists offer treatments like physical therapy, joint injections, medications, and other techniques to reduce pain and restore movement. Every care plan is tailored to your individual needs.
In the past year, our team provided comprehensive orthopedic care through both clinic visits and surgical services.
Our surgeons treated a wide range of conditions, this past year, including joint replacements and trauma-related injuries.
Some patients go home the same day, while others need more time. This average reflects our focus on efficient care and steady recovery.
Our dedicated, collaborative team is committed to providing exceptional orthopedic care in Coos Bay and across Oregon’s South Coast.

Dr. Vallier brings the kind of experience you can only earn under pressure. His medical path began in Berkeley and continued at Loyola University of Chicago Stritch School of Medicine, and orthopedic training in San Francisco while serving in the Army. He went on to care for injured service members in Germany and during Operation Desert Storm in Saudi Arabia.
After nearly two decades of practice in Yuba City, he returned to Oregon in 2012 and is proud to call it home. His military background shaped his focus on sports injuries, trauma care, and joint replacement, experience he now brings to patients across the region.
When elite athletes need care, they call doctors like Dr. Van Sice. With nearly two decades in orthopedic care, he has treated professional athletes from teams like the LA Kings, LA Lakers, LA Dodgers, and Miami Marlins, as well as collegiate football programs. He earned his medical degree from Tulane University School of Medicine, where he later served as an assistant professor of orthopedic surgery.
In addition to sports medicine, he has expertise in treating arthritis and other joint conditions. Recognized for excellence in both damaged ligaments and tendons of the shoulder, elbow, and knee with minimally invasive techniques, arthritis, and other joint conditions in academic and clinical settings, Dr. Van Sice is proud to be back in his home state. He’s a graduate of Warrenton High School on Oregon’s north coast.


Greg Sopka, PA has built his career helping patients move better. He specializes in musculoskeletal health and injury rehabilitation, supporting recovery from strain, overuse, or orthopedic injury. After earning his Bachelor of Science from the University of Detroit Mercy, he completed his Master’s in Physician Assistant Studies at Ohio Dominican University.
Greg is known for his collaborative, patient-focused care and plays a key role in diagnosis, treatment planning, and recovery support across the orthopedic team.
When things get complex, Stephanie Perez, PA is who surgeons trust. She specializes in orthopedic surgical assistance, trauma care, and joint injections and aspirations. After earning her BA in Biopsychology with a Chemistry minor from Monmouth College, she completed her Master of Physician Assistant Studies at St. Ambrose University.
Stephanie is NCCPA certified and holds Advanced Cardiac Life Support certification. She brings a steady presence and sharp clinical skills to every phase of surgical care.

We provide our patients with support throughout their treatment experience through our Nurse Navigator Program. You’ll be assigned a Registered Nurse that will work directly with you to promote your recovery. They will work directly with you to:
Nurse Navigator specializing in patients undergoing knee and hip replacements.
Nurse Navigator specializing in knee and hip replacements, injuries, sports injuries, and surgeries.

Pain and injuries are enough to deal with on their own. That’s why we accept most major insurance providers and offer convenient Bay Area locations with flexible appointment times, so you can focus on your health, not the hassle.
Ready to take the next step? Our orthopedic team is here to help you move better and live well.
Request your appointment below. We’ll be in touch soon.
(541) 269-8111
1775 Thompson Rd, Coos Bay, Oregon 97420

(541) 266-7846
(541) 269-8502 FAX
Have a question? We’re here to help. Explore our patient education guides, get quick answers about care, recovery, and what to expect, or reach out to us directly.
Pre-Operative Total Knee Replacement education
Pre-Operative Total Hip Replacement education
How long will I be in the hospital?
Your length of stay depends on the goals to be accomplished and how you progress after surgery. Certain goals will need to be accomplished before you go home, like walking with minimal assistance and pain managed on oral pain medications. Some patients may discharge the same day as their surgery while others may have a one-night stay. Your discharge will be when it’s clinically appropriate.
When will my family or friends be able to see me after surgery?
Your family and friends can wait in the family waiting areas until you are settled in your room and all nursing assessments needed are completed. Rest is essential and is frequently interrupted by hospital staff. You can request “No visitors,” even if it’s for only a short time during your day. Family members or friends who are ill should wait to visit until they feel well again. All visitors should wash or sanitize their hands. We realize the importance of family and friends’ support for your social and emotional well-being. Your room has been designed to accommodate them.
What transportation will I need to go home from the hospital?
You may go home in a private vehicle of your choice. Be sure the vehicle has plenty of legroom and a reclining seat that is not too high or too low to get in and out of safely. You will need assistance with transfers in and out of the vehicle until you are stronger and can do more for yourself. Local transportation services to home are available. There is a fee for this service. Let your nurse or discharge planner Orthopedic Navigator know if you would like this arranged.
How do I obtain the necessary equipment needed for activity and home use?
Your occupational therapist will give you tools for activities of daily living while you are in the hospital. However, if you need a front wheeled walker or a raised toilet seat, you may want to shop the thrift stores. Not all insurance companies, including Medicare, cover equipment needs, so know your benefits. If you don’t have what you need by the time you have surgery, your case manager Orthopedic Navigator can assist in options on how to obtain this equipment.
I have steps or stairs at home. Who will teach me to go up and down them?
Your physical therapist will teach you how to safely climb up and down steps or stairs. If your home environment has steps or stairs, you may want to modify your living situation, so you do not have to climb up and down steps or stairs on a daily basis.
How soon will I be able to return to normal daily activities?
You will have a modified lifestyle during the first six weeks with limited activities and can return to normal daily activities within three to six months.
When will I be able to drive?
Certain activity restrictions may prevent you from driving safely. Until these restrictions are no longer a consideration, you will need to have someone drive you to your appointments. Talk with your surgeon during your follow-up appointment.