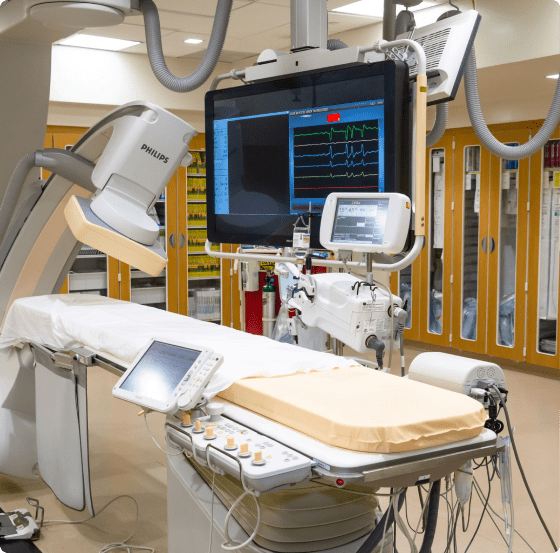
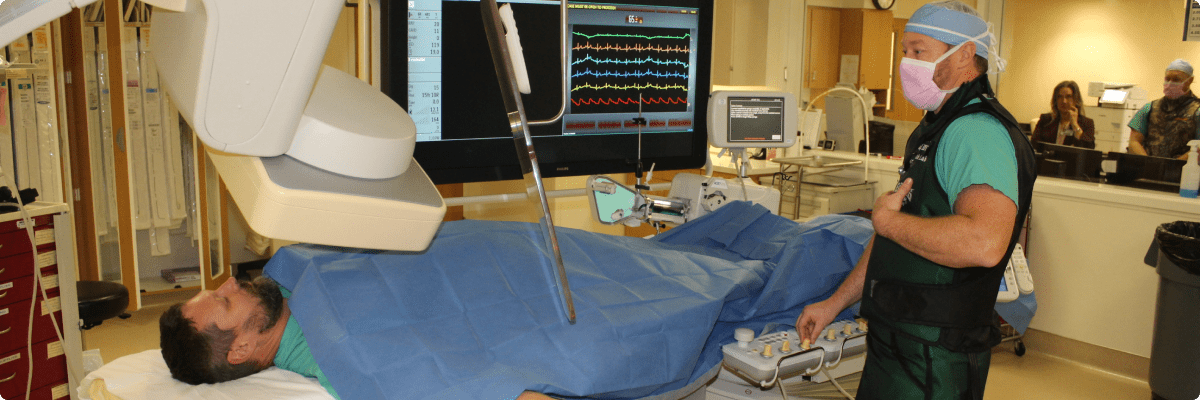
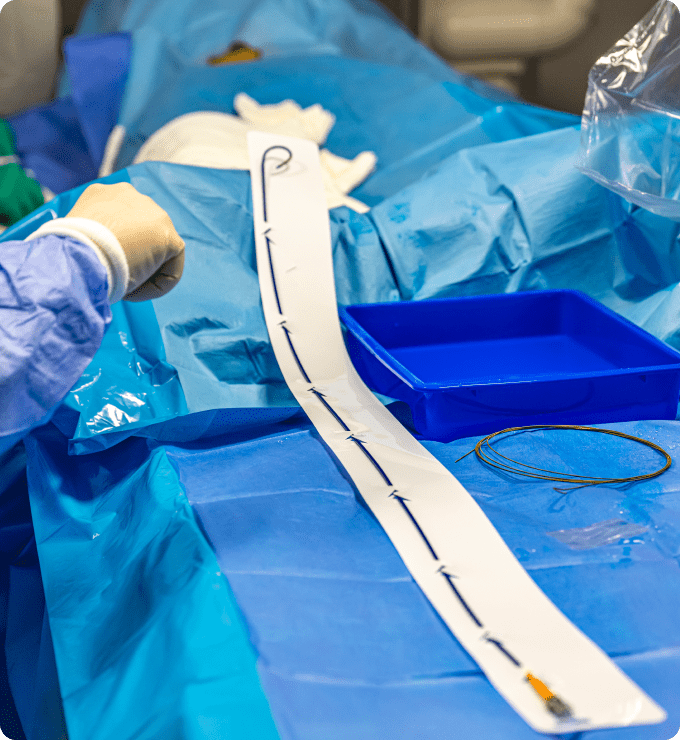
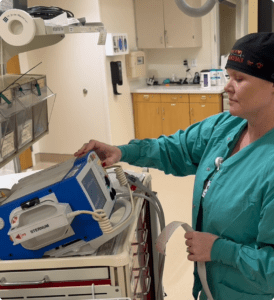
Impella pumps, like the one used to save Kurt’s life, are not commonly used, and they are reserved for the very worst cases. It’s also an expensive device for a hospital to purchase, so many facilities don’t have one at all. Fortunately, the stars were aligned for Kurt, and the pump was able to move the blood and oxygen to all of his organs, so he not only survived, he thrived.
After a few days, Kurt’s condition had improved to the point where the Impella pump could be removed, but all the lifesaving CPR had taken a toll on his ribs: many were cracked or broken, and Kurt was suffering from flail chest, a life-threatening condition that occurs when a segment of the rib cage breaks due to trauma and becomes detached from the rest of the chest wall. Kurt was transferred to Oregon Health & Science University to have his chest plated, but prior to the procedure a CT scan found more than just damaged ribs. The odds had been stacked against Kurt from the beginning, and now kidney cancer was in the mix. Kurt’s chest was plated, and he was on his way to recovery.
“I’ve got a pile of metal in me and 52 screws, so I’ve got a small erector set in there,” he says.
Kurt reaches into his pocket for his phone and pulls up a video of his time in the hospital after heart surgery. Tubes trail from his open mouth and nostrils, and his face is drained of color. He looks motionless, aside from the slow rise and fall of his chest.
“That was me,” he says, pausing for a moment. “I don’t remember any of that.”