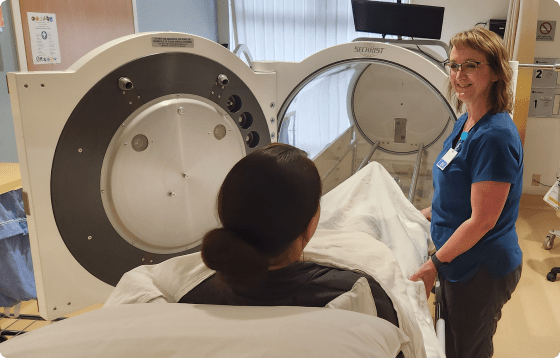
Wound and Hyperbaric
Center
Advances in medical science are helping more people than ever survive serious illnesses. However, people who survive heart attacks, diabetes, or other chronic conditions may be weakened and less able to heal wounds. Effective wound care is increasingly important in maintaining these patients’ quality of life. Bay Area Hospital provides a comprehensive outpatient evaluation and management program.